The Shea Clinic offers a world-class inner ear medication delivery program for treatment of Meniere’s disease, sudden sensorineural hearing loss, and other forms of inner ear disease. Our perfusion protocols have been developed over decades as the Shea Clinic was one of the pioneering centers in the world at developing techniques to deliver medications to the inner ear in the 1980s and 1990s. Our approach is not only grounded in published research, but it is also based on the collective long-term experience of the clinic in treating tens of thousands of patients over the last few decades. Our quality-based approach to inner ear perfusion is uniquely excellent and only rarely duplicated elsewhere.
What is an Intratympanic Perfusion?
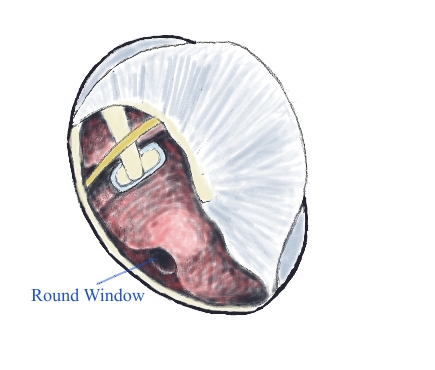
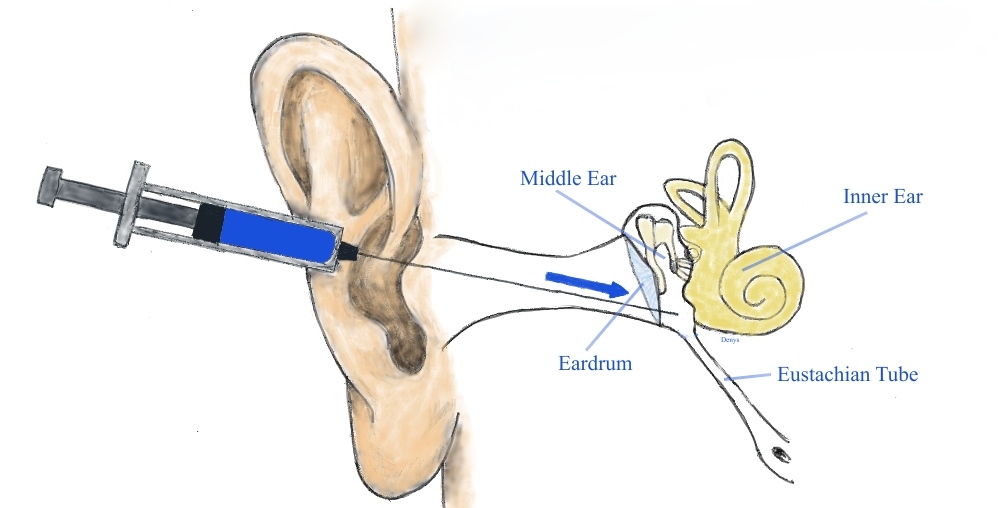
Intratympanic perfusion is a method of delivering medication to the innermost part of the ear, where the organs of hearing and balance are located. It is currently not feasible to safely inject medications directly into the inner ear, so perfusion techniques were developed to overcome this limitation by delivering medication via an indirect route. Intratympanic perfusion involves injecting medication into the middle ear space (located behind the eardrum) using a very fine needle. From there, the medication will diffuse into the inner ear over time by passing through the tiny permeable membrane (called the round window) that separates the inner ear from the middle ear space.
Perfusion therapy has a few unique advantages:
- Reaches higher medication concentrations in the inner ear than is achieved by taking medications by mouth or through an IV
- Provides a way to target a single inner ear while avoiding treatment of the opposite ear (when desired)
- Limits absorption of medication into the bloodstream, thereby minimizing drug-related side effects to the rest of the body, which is desirable in some situations, i.e. diabetes
Although inner ear perfusion has been routinely performed in clinics around the world for a few decades, including most every major hospital with an Ear, Nose, Throat (otolaryngology) department, there are no medications currently approved by the US Food & Drug Administration for injection into the ear for any specific ear disease; as such we rely upon the vast experience of our clinic to determine when and how this is indicated in joint discussion with our patients.
Five Aspects That Make the Shea Clinic Perfusion Program Uniquely Excellent
- Drug Concentration:
The two main classes of medications used for perfusion therapy are steroids and aminoglycosides.
- Steroids are anti-inflammatory medications. The steroid used in our program is dexamethasone, which is among the most potent medications in the steroid class in terms of anti-inflammatory effect. In addition to relieving inflammation, steroids also appear to impact fluid channels within the inner ear (aquaporins) that play a role in inner ear fluid homeostasis and fluid pressure regulation. Steroids are particularly effective in the treatment of Meniere’s disease and sudden sensorineural hearing loss.
When performing intratympanic steroid perfusions, our aim is to apply very high drug concentrations, typically using a solution of 24 mg/ml of dexamethasone. This is higher than the commercially mass-produced dexamethasone solutions of 4 or 10 mg/ml, which are commonly used. Acquiring this high steroid concentration requires collaboration with a specialized compounding pharmacy. Our goal at the Shea Clinic is to maximize the amount of steroid that enters the inner ear so as to induce the greatest possible anti-inflammatory effect.
- Gentamicin and streptomycin are antibiotic medications in the class known as aminoglycosides. In addition to their use in treating infection, they also impart permanent biochemical effects on the inner ear, and this property is used to manage inner ear disease. Gentamicin, which is the most commonly used aminoglycoside in the current era, is useful when the balance portion of the inner ear is hyperactive or abnormally stimulated, which may cause vertigo or imbalance. The concept of gentamicin perfusion can be thought of as having an irreversible “numbing” effect on some of the balance receptors in the inner ear, which in turn renders the ear less sensitive to excessive stimulation and therefore less likely to make a patient feel dizzy. This is very effective at “blunting” the most severe of the vertigo attacks associated with Meniere’s disease.
The most common indication for gentamicin perfusion is management of Meniere’s disease when less aggressive therapy has failed to control severe recurrent vertigo attacks, but it may also be used to treat other inner ear conditions. When indicted, perfusion of the ear with gentamicin is highly effective (>90%) at controlling severe vertigo spells caused by Meniere’s disease. Intratympanic therapy has reduced the need for more invasive procedures like endolymphatic sac decompression/shunt (surgically draining the inner ear to relieve pressure), vestibular nerve section (cutting the balance nerves between the inner ear and the brain), and labyrinthectomy (surgically removing the balance organs of the inner ear).
A large-scale study of streptomycin perfusion for the treatment of Meniere’s disease performed by Paul F. Shea MD, FACS at the Shea Clinic found that streptomycin perfusion had a high rate of improvement in quality of life and a low rate of hearing loss.
In contrast to steroid perfusions, our aim for gentamicin perfusion is to deliver the lowest effective dose. We titrate our dosing according to individual patient needs and observed treatment response, so as to minimize the risk of side effects. Potential side effects of gentamicin perfusion include worsened hearing in the treated ear (most patients already have significant hearing loss prior to gentamicin perfusion due to the effects of their Meniere’s disease) or prolonged imbalance after treatment. In our opinion, over-dosing of gentamicin can be a problem if the unique pharmacology and behavior of this medication in the ear is not properly accounted for in dose planning.
- Hyaluron Gel Vehicle (Solution):
Our intratympanic medications are prepared into a gel-like form by combining them with a medium called hyaluron (hyaluronic acid), which has been established to be completely safe for middle ear application. Hyaluron gel has a thickening effect that holds the medication in the space behind the eardrum over a longer period of time as compared to mass-produced water-based steroid or gentamicin solutions that may exit the middle ear into the back of the throat very shortly after application in the office.
More importantly, hyaluron greatly increases the permeability of the tiny membrane (round window) that separates the middle ear from the inner ear and has been proven to increase the inner ear drug concentrations achieved during perfusion as compared to standard water-based solutions. In fact, intratympanic perfusion with water-based steroid solutions result in inner ear concentrations that peak within a few hours after application but then almost completely “wash out” within 24 hours. In contrast, perfusion with steroid in hyaluron gel yields higher peak inner ear drug concentrations as well as drug levels that persist in the inner ear for a few days.
This graph shows the difference between inner ear steroid concentration over time for 10 mg/ml of hyaluron/steroid (Blue) versus standard 10 mg/ml of water-based steroid injection (Yellow). The water-based solution is washed out after 24 hours (red arrow) while the hyaluron/steroid persists much longer.
- Perfusion Timing:
We typically perform intra-tympanic steroid perfusions on three successive days. It is common practice in the field of otology to perform multiple drug perfusions as part of a series spaced days to weeks apart, yet it is our opinion that the very specific timing of perfusions is important. For steroid perfusion, a higher peak inner ear concentration is achieved if the second and third perfusions are performed during a window of time where there is still drug persisting from the preceding day(s) perfusions. In other words, the second and third perfusion concentrations should “piggy back” on the prior day’s dosage resulting in stair step increase in peak concentration in the inner ear.
This graph portrays the effect of “piggy-backing” steroid injections in hyaluron base on 3 successive days. The first day (blue) is still present when the second day’s dose is applied (orange). Likewise, the first- and second-days’ dose are still present when the third day’s dose is applied (grey). Note the progressive stair step increase in peak dosage (red arrows).
For gentamicin perfusion, timing is more complex. Depending on a patient’s particular clinical situation, it is often desired to space each successive perfusion out by 4-6 weeks. This is because there is usually a delay of several days between the point when gentamicin is applied to the ear and the point when it starts to exert intended effects on the ear. In such cases, we may allow time to assess the impact of each perfusion before proceeding with another in order to avoid over-dosage.
- Thoroughness and Patient Comfort:
We believe that optimizing a patient’s comfort during perfusions may improve outcomes. Because perfusion may sometimes cause mild discomfort, our patients receive a low dose of sedative medication via an IV prior to their perfusion in order to help them relax and tolerate the process comfortably. To safely do this, we perform our perfusions in a specialized outpatient surgical facility. After medication is applied to the ear, patients rest in mildly sedated comfort while lying on their side for approximately 2 hours while the medication is thoroughly absorbed. When multiple perfusions are planned, the IV placed for the first perfusion is left in place until after the third perfusion is completed two days later, so the IV only has to be placed one time.
It is important to acknowledge that this aspect of the Shea Clinic perfusion program is quite different from standard practice at the overwhelming majority of centers that perform inner ear drug perfusion. The common practice elsewhere is to simply inject medication in the office without sedation, and then have the patient wait for 20-30 minutes while reclined in an office chair. Although that approach is indeed simpler, we believe it is also less thorough, less comfortable, and less consistent than our method. We can only offer this to our patients because of the historical legacy of the Shea Clinic as a pioneering center of excellence and innovation in the field of otology that brought about the existence of our outpatient surgery center infrastructure that is able to support a specialized intratympanic perfusion program.
- Minimizing the Risk of a Hole in the Eardrum:
Although uncommon, acquiring a hole in the eardrum is the most common complication of inner ear drug perfusion. Other rare complications include worsening hearing loss, persistent dizziness or imbalance, ringing in the ear, and ear infections. Because our perfusions are performed in a controlled setting with the patient sedated, we are able to avoid the need to apply harsh numbing medications such as phenol to the eardrum, as is common elsewhere. We believe that repetitive application of medications such as phenol may increase the risk of developing a hole in the eardrum. At the Shea Clinic, the rate of perforation after perfusion therapy has been less than 1% from many thousands of perfusions performed over the last few decades.
Inner ear perfusion therapy is generally covered by commercial insurance and by Medicare. We accept patients for intratympanic perfusion from all over the USA and abroad into our program. For those wanting to come to our facility for perfusions, we have a “Shea discount” agreement with an adjacent hotel and we seek to make the out-of-network or self-pay process easy and feasible.
References:
- Borden RC, Saunders JE, Berryhill WE, Krempl GA, Thompson DM, Queimado L. Hyaluronic acid hydrogel sustains the delivery of dexamethasone across the round window membrane. Audiology and Neurotology. 2011;16(1):1-1.
- Casani AP, Piaggi P, Cerchiai N, Seccia V, Sellari Franceschini S, Dallan I. Intratympanic treatment of intractable unilateral Meniere disease: gentamicin or dexamethasone? A randomized controlled trial. Otolaryngology–Head and Neck Surgery. 2012 Mar;146(3):430-7.
- Gluth MB. On the Relationship Between Menière’s Disease and Endolymphatic Hydrops. Otology & Neurotology. 2020 Feb 1;41(2):242-9.
- Fukushima M, Kitahara T, Uno Y, Fuse Y, Doi K, Kubo T. Effects of intratympanic injection of steroids on changes in rat inner ear aquaporin expression. Acta oto-laryngologica. 2002 Jan 1;122(6):600-6.
- Garduño-Anaya MA, De Toledo HC, Hinojosa-González R, Pane-Pianese C, Ríos-Castañeda LC. Dexamethasone inner ear perfusion by intratympanic injection in unilateral Meniere’s disease: a two-year prospective, placebo-controlled, double-blind, randomized trial. Otolaryngology—Head and Neck Surgery. 2005 Aug;133(2):285-94.
- Han X, Yin X, Du X, Sun C. Combined intratympanic and systemic use of steroids as a first-line treatment for sudden sensorineural hearing loss: a meta-analysis of randomized, controlled trials. Otology & Neurotology. 2017 Apr 1;38(4):487-95.
- Postema RJ, Kingma CM, Wit HP, Albers FW, Van Der Laan BF. Intratympanic gentamicin therapy for control of vertigo in unilateral Meniere’s disease: a prospective, double-blind, randomized, placebo-controlled trial. Acta oto-laryngologica. 2008 Jan 1;128(8):876-80.
- Salt AN, Plontke SK. Local inner-ear drug delivery and pharmacokinetics. Drug discovery today. 2005 Oct 1;10(19):1299-306.
- Selivanova OA, Gouveris H, Victor A, Amedee RG, Mann W. Intratympanic dexamethasone and hyaluronic acid in patients with low-frequency and Meniere’s-associated sudden sensorineural hearing loss. Otology & Neurotology. 2005 Sep 1;26(5):890-5.
- Shea JJ. Perfusion of the inner ear with streptomycin. The American journal of otology. 1989 Mar 1;10(2):150-5.
- Shea JJ, Norris CH. Streptomycin perfusion of the labyrinth. Acta Oto-Laryngologica. 1991 Jan 1;111(sup485):123-30.
- Shea Jr JJ. Classification of Menière’s disease. The American journal of otology. 1993 May 1;14(3):224-9.
- Shea Jr JJ, Ge X. Dexamethasone perfusion of the labyrinth plus intravenous dexamethasone for Ménière’s disease. Otolaryngologic clinics of North America. 1996 Apr 1;29(2):353-8.
- Shea JJ. The role of dexamethasone or streptomycin perfusion in the treatment of Meniere’s disease. Otolaryngologic Clinics of North America. 1997 Dec 1;30(6):1051-9.
- Shea PF, Richey PA, Wan JY, Stevens SR. Hearing results and quality of life after streptomycin/dexamethasone perfusion for Meniere’s disease. The Laryngoscope. 2012 Jan;122(1):204-11.
- Stokroos R, Kingma H. Selective vestibular ablation by intratympanic gentamicin in patients with unilateral active Ménière’s disease: a prospective, double-blind, placebo-controlled, randomized clinical trial. Acta oto-laryngologica. 2004 Mar 1;124(2):172-5.
When you lose your hearing, those around you suffer the most.
Connect with your loved ones

